Everyone’s experience of having a baby is different and knowing when to seek help can be confusing.
How long should I wait?
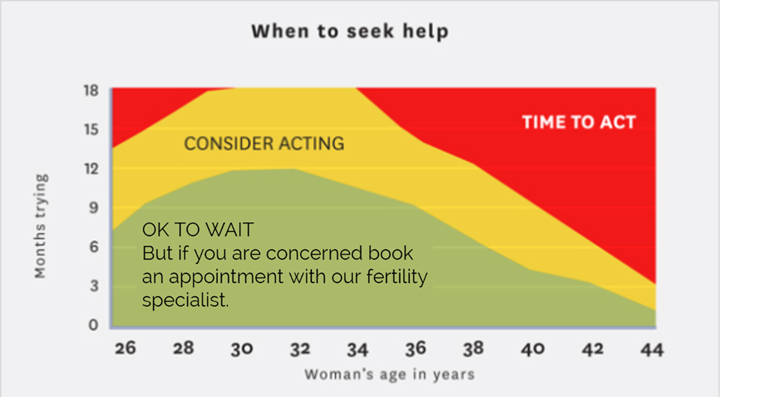
As fertility declines with age, your biological clock is the most important factor to consider.
The graph below shows the recommended time frames for trying to conceive naturally before seeking help. For example, if you are 39 years old you should consider seeking help after 5 months, and should definitely be seeking advice after 1 year.
You can check where you sit on the graph and your specific timeframes using the biological clock.
For more information about fertility and the biological clock, visit our ‘How age affects fertility’ page.
When to seek advice early
- If you have polycystic ovaries, endometriosis, or have been through a cancer diagnosis; we recommend you get in touch quickly so we can talk you through all your options and give you the greatest possible chance of success.
- If you’re a single woman considering motherhood in the future; it’s best to approach us early and consider egg freezing as this can be an option for you while you have a higher ovarian reserve and healthier eggs. More here

